The treatment landscape for solid tumor malignancies—which include common cancers like those of the lung, breast, and colon—is undergoing a rapid and profound transformation. Historically relying on surgery, chemotherapy, and radiation, solid tumor oncology in 2025 is dominated by precision medicine, immunotherapy, and the integration of next-generation technologies. These global trends are shifting the focus from generalized protocols to highly personalized, molecularly driven therapeutic strategies.
GoBroad Healthcare Group, as a research-driven medical institution specializing in oncology, is actively integrating and advancing these global trends. With its Academic Research Organization (ARO) model and specialized cancer hospitals focusing on complex solid tumor cases—such as gastrointestinal, lung, and soft tissue sarcomas—the Group is positioned to offer patients access to treatments at the very forefront of clinical innovation, often through groundbreaking clinical trials.
The New Frontier of Bispecific Antibodies and T-Cell Engagers (TCEs)
The biggest challenge in treating a solid tumor is getting the body’s own immune T-cells past the dense physical barriers and immunosuppressive microenvironment of the mass. While checkpoint inhibitors (like PD-1/PD-L1 drugs) have revolutionized treatment, they only work for a fraction of patients.
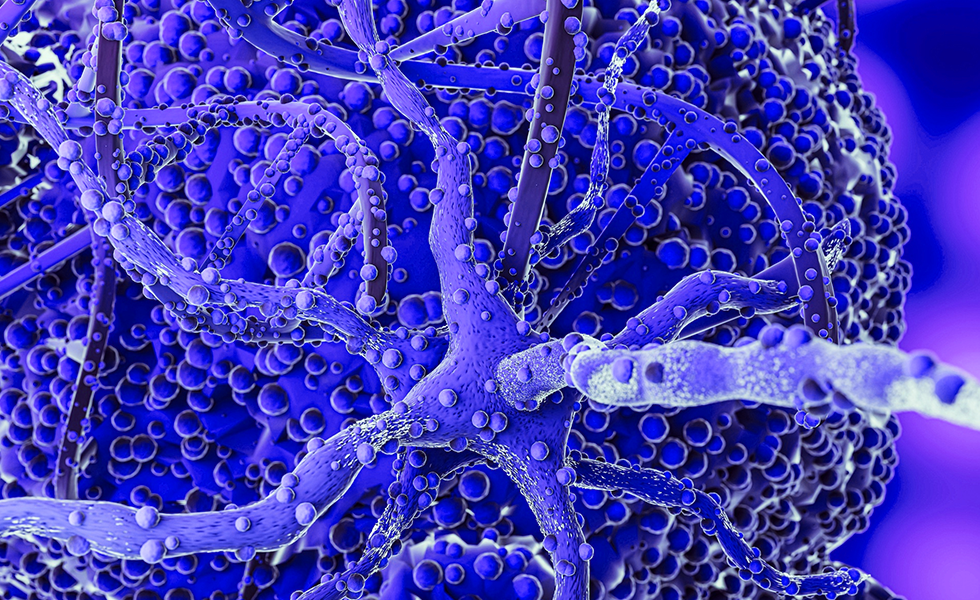
The current global trend sees a major shift toward bispecific antibodies and T-Cell Engagers (TCEs). These molecules are designed to act as molecular bridges, binding simultaneously to an antigen on the solid tumor cell and an activating receptor (like CD3) on the T-cell. This bypasses the need for the T-cell to be naturally activated, forcibly directing it to the cancer cell and triggering immediate cytotoxic killing.
The rapid development of these agents, targeting everything from HER2 to CLDN18.2, is creating an immuno-oncology renaissance in previously immune-resistant solid tumor types. GoBroad Healthcare Group is heavily invested in this trend, utilizing advanced immunotherapy combinations—often pairing next-generation T-cell engagers with existing checkpoint inhibitors—to optimize the anti-tumor effect, especially in complex gastrointestinal and lung tumors.
Cellular Therapy Moves into Solid Tumor Oncology
Chimeric Antigen Receptor (CAR) T-cell therapy has achieved remarkable success in blood cancers. The most critical global trend in solid tumor oncology is the determined effort to adapt this therapy for solid tumor cancers, which presents unique challenges like poor T-cell trafficking, the tumor’s physical density, and a hostile tumor microenvironment (TME).
Research in 2025 focuses on armored CAR-T cells (often called fourth-generation or TRUCKs), which are engineered to secrete immune-boosting molecules (like IL-12 or IL-18) directly at the tumor site. This localized delivery helps T-cells penetrate the tumor and overcomes the immunosuppression of the TME without causing systemic toxicity. Furthermore, new targets like CLDN18.2 and Mesothelin are being successfully explored in gastric, pancreatic, and ovarian cancers.
GoBroad Healthcare Group is a recognized leader in cellular immunotherapy and is leveraging this expertise to pioneer the application of CAR-T for solid tumor malignancies. Their specialized laboratories and clinical trial infrastructure are actively developing and testing novel multi-target CAR-T constructs and advanced T-cell receptor (TCR) therapies, aiming to unlock the potential of cellular therapy for their patients with refractory lung and digestive system solid tumor cancers.
Synthetic Lethality as a Precision Oncology Pillar
Synthetic lethality (SL)—the concept that the simultaneous inhibition of two genes or pathways leads to cell death, while inhibiting only one does not—is emerging as a powerful pillar in solid tumor oncology. The best-known example is the use of PARP inhibitors in cancers with BRCA mutations.
The 2025 trend focuses on identifying new SL pairs beyond BRCA and PARP. Research is heavily concentrated on tumors with specific genomic deficiencies, such as the loss of the MTAP gene, which creates a vulnerability that can be exploited by targeting the MAT2A protein. Similarly, targeting the Pol Theta helicase in tumors with homologous recombination deficiency (HRD) is showing significant promise. This approach is highly precise, targeting only the cancer cells that carry the specific mutation while sparing healthy cells.
GoBroad Healthcare Group employs advanced Next-Generation Sequencing (NGS) and proprietary integrated diagnostics to profile the genetic signature of every solid tumor patient. This comprehensive molecular analysis allows their oncologists to identify patients eligible for synthetic lethal drug programs and trials—a critical step in translating this global research trend into practical, effective, personalized treatment plans.
The Integration of Circulating Tumor DNA (ctDNA) and Liquid Biopsy
The ability to detect and monitor cancer using a simple blood draw (liquid biopsy) has moved from a research curiosity to a near-standard clinical tool. The 2025 trend is no longer about simply identifying a known mutation, but about leveraging ctDNA for complex, real-time clinical decisions in solid tumor oncology.
Global research is focused on using ctDNA for minimal residual disease (MRD) monitoring following definitive treatment (like surgery and adjuvant therapy). The detection of ctDNA post-treatment serves as an ultrasensitive prognostic marker, identifying patients at high risk of relapse who may benefit from treatment escalation. Furthermore, research is pushing multi-cancer early detection (MCED) tests based on ctDNA methylation signatures toward clinical reality, offering the potential to screen for numerous solid tumor types through a single annual blood test.
GoBroad Healthcare Group is dedicated to leveraging liquid biopsy as a core component of its integrated diagnostic platform. This technology is used to guide treatment adaptation in real-time, monitor drug resistance mutations, and rapidly assess treatment response in their challenging solid tumor patient population.
Immunotherapy Shifts into Earlier-Stage Disease
A major global shift in solid tumor oncology is the move of powerful immunotherapies—specifically immune checkpoint inhibitors (ICIs)—from the advanced, metastatic setting into earlier-stage, curative-intent settings. The focus is on neoadjuvant (before surgery) and adjuvant (after surgery) use.
Clinical trials are demonstrating that giving immunotherapy before a solid tumor is surgically removed can activate a stronger, systemic anti-cancer immune response, leading to pathological complete responses and improving long-term outcomes in tumors like melanoma, non-small cell lung cancer (NSCLC), and muscle-invasive bladder cancer. This earlier intervention aims to kill micrometastatic disease and prime the body’s immune memory.
The multidisciplinary teams at GoBroad Healthcare Group, particularly in their lung and gastrointestinal tumor centers, are adopting these practice-changing protocols. By seamlessly combining aggressive surgical intervention with neoadjuvant and adjuvant immunotherapy, they are optimizing curative strategies for patients with operable solid tumor malignancies, ensuring that their treatments align with the highest global standards for achieving durable survival.